


Shoulder Instability
Shoulder is the most common joint in the body to dislocate. Due to its inherent design we have a great deal of mobility within the shoulder, which is directly at the cost of stability. Shoulder instability may present as repeated dislocation where in, patent has to go to a hospital to relocate the shoulder – often under sedation. Sometimes patients are able to relocate their shoulder
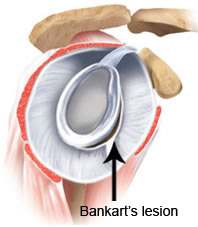
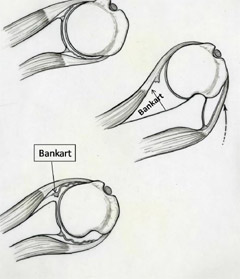
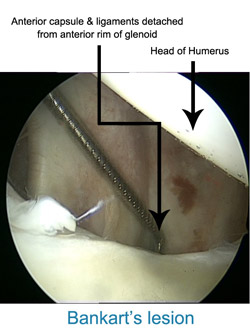
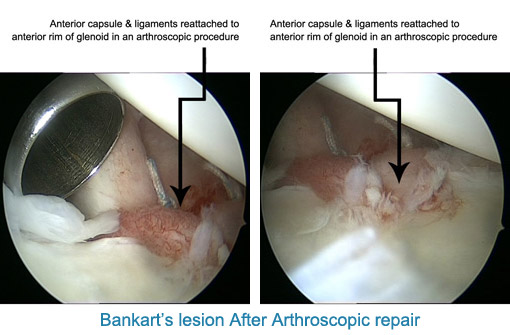
themselves. Shoulder dislocation is a recurrent phenomenon. Commonly after the first dislocation there is a risk of 60% - 90% recurrence. If the shoulder dislocated again there is more than 90% chance that it will re-dislocate. Each time the shoulder dislocated it peels off the attached ligament (Labrum) worsening the damage. Along with the ligament, the cartilage of the joint on both sides (Glenoid & Humerus) is damaged permanently. Cartilage damage cannot be repaired and is a permanent feature.
It is prudent to get treated early to avoid long-term problems. Repeated shoulder dislocations can lead to nerve injury, which may heal incompletely. Repeated peeling of the cartilage will eventually lead to early arthritis which can be disabling and compromise daily essential activities.
In the past the surgery for recurrent dislocation was open surgery sometimes with a hideous scar & mixed results. In the modern era, few hospitals are geared to treat this condition, with Arthroscopic repair by the name of Bankart repair. The Keyhole surgery leaves three small puncture wounds. Patient goes home the next day of surgery and usually resumes light work in few days. Patient must avoid driving for 2 months after surgery. By three months most patients have achieved their full range of movement & strength. The results of Arthroscopic Bankart repair at our practice have been impressive with so far no patient has dislocated shoulder after surgery hence therefore no patient requiring revision surgery.
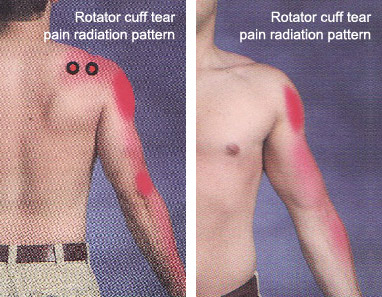
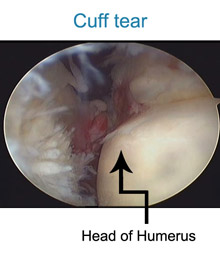
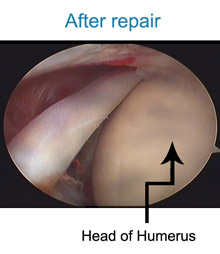
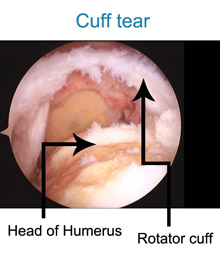
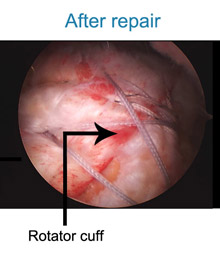
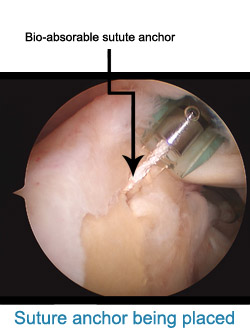
The rotator cuff muscle is a prime muscle in stabilizing the shoulder joint & allows us to lift the arm above the head. Due to wear & tear over time, it is common in patients above age of 50 years to develop a rotator cuff tear. Often this tear occurs without any fall or trauma. However sometimes due to prevailing degeneration within the rotator cuff, a trivial trauma- such as fall in bathroom or a throwing injury may lead to a tear. Patients complain of pain at the side of the arm and inability to actively lift the arm. The rotator cuff tear can be diagnosed either by ultrasound or MRI examination. If there is a partial tear, this can be treated by our shoulder rehab program. However, once a full thickness tear occurs, it can only be treated by surgical repair. Without repairing the tear, the shoulder cannot gain function. Local heat or physiotherapy does not address the cuff defect. Untreated, the tear will propagate with time and a late presentation leads to a poor outcome. Some patients have to be refused surgery as the tear becomes irreparable. In that situation reverse shoulder replacement remains the only valid option. Traditionally rotator cuff used to be repaired with open surgery leading to adhesions and post operative stiffness & recovery generally took a long time. At our clinic rotator cuff is repaired arthroscopically with the use of imported suture anchors. After arthroscopic repair, patients goes home the next day of the surgery & with hardly any scar.
Also , working patients tend to join back work with in a week of surgery. So far we have hardly had complications with arthroscopic repair. In our series the chance of re-tear, especially with patients presenting early , is less than 1 % . Patient presenting late will tend to have a poor quality of muscles to repair. We have the largest series of arthroscopic rotator cuff repair patients, with best clinical outcome and longest follow-up.
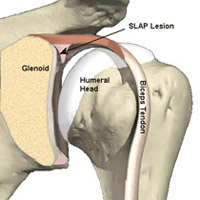
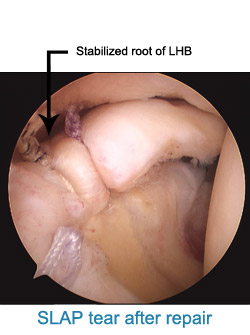
SLAP tear is an acronym for SUPERIOR LABRUM ANTERIOR TO POSTERIOR tear. These are seen classically in athlete’s involved in throwing activities. In the routine non-athlete, the tear occurs following a jerk to the shoulder- like falling from height, jerk from a dog leash or when holding the overhead bar when traveling in a local bus.
SLAP tears are often missed, as they can be difficult to diagnose. One can diagnose SLAP tears clinically but have to be confirmed by MRI at a standard centre. Minor Grade I SLAP tears may be treated with rehabilitation. However frank SLAP tears, which are full thickness tears- Grade II, III or IV, will need surgical repair.
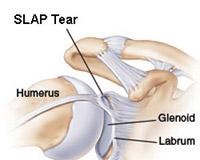
Open surgery is not an option for treatment of SLAP tears.
Arthroscopic repair remains the only solution. Only three
small puncture scars are made & patients go home the
next day of surgery. They can join back work within a
week. Once repaired effectively, SLAP tear heals up in six
weeks. After this, patient attends a two-week supervised
shoulder rehab program. Those who are sportsman may resume
their sports activities not before 4-6 months after
surgery.
We have had several national athletes, including cricket’s
players, wrestlers, weight lifters, national javelin
throwers, who have gone back to their sports.


Stiff shoulder also known as frozen shoulder or adhesive capsulitis is a complex condition which is less understood all over the world. In my practice we prefer to treat most of the patients with stiff shoulder with our excellent rehab program. Patient typically attends our unique exercise program and is supervised for two weeks back to back. They are assessed for improvement in range of movement, pain relief and strength gain at the end of two weeks. If they are 50% better, they qualify to go on a home program for next 6-8 weeks. More that 85% patients improve with this regime. The program is a novel and unique combination of thera band exercises and range of movement restoration. We prefer not to prescribe pain killer or mechanical modalities like ultrasound or shortwave diathermy or IFT. The idea is to initiate an improvement which the patient can then sustain by practicing at home.
Patient that come late or with severe grade III stiffness may respond sub optimally to the rehab program and may need surgery for the same. We perform this rarely. No patient is offered surgery for this condition unless he has done trial of rehab before. In such patient we perform a arthroscopic adhesiolysis. This involves key-hole surgery where we release the adhesions which are cord like stiff bands which are responsible for constraining the movements of the shoulder join. This involves resecting the CHL ligament , anterior and posterior capsule, along with subacromial decompression. Patients are given a nerve block for pain relief which last for about 10-12 hours. Or more recently we place an intra-articular catheter for post-operative analgesia. Patients are discharged the very next day after the surgery. None of our patients complain of pain by evening on surgery day. Patient start there rehab program from first day of surgery. Pain relief if quick to come, however, restoration of range of movement can take few weeks depending upon pre-operative severity & duration of stiffness.
Finally all our patients regain near full range of motion at the shoulder joint.
Severe restriction of movement at right shoulder

Full range of movement restored at right shoulder after arthroscopic release of capsular adhesions
