Osteotomy literally means "cutting of the bone." In high
knee osteotomy, the tibia (shinbone) is cut and then
reshaped to relieve pressure on the medial compartment of
knee joint. It is used when you have early-stage
osteoarthritis that has damaged just one side of the knee
joint. By shifting your weight off of the damaged side of
the joint, an osteotomy can relieve pain and significantly
improve function in your arthritic knee.
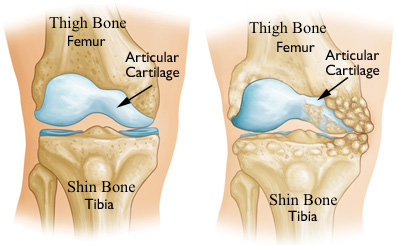
Why does arthritis affect one side of the joint?
Medial osteoarthritis can develop when the bones of your
knee joint do not line up properly. This is a common
situation in Asian sub-continent, as people of this region
genetically have varus knee alignment. This can put extra
stress on the inner (medial) side of your knee. Over time,
this extra pressure can wear away the smooth cartilage that
protects the bones, causing pain and stiffness in your knee.
A trivial incidence of trauma to the knee joint can
aggravate the process of medial joint wear out.
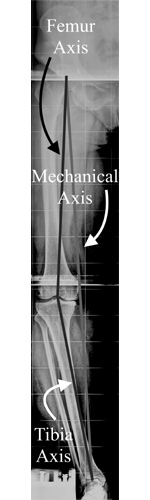
Goals of High Tibial Osteotomy
To transfer weight from the arthritic medial compartment of
the knee to a healthier lateral compartment by correcting
the alignment of knee joint, thus prolonging the life span
of the knee joint.
Advantages and disadvantages of HTO
By preserving your own knee anatomy, a successful osteotomy
may delay the need for a joint replacement for several
years. Another advantage is that there are no restrictions
on physical activities after an osteotomy - you will be able
to comfortably participate in your favorite activities, even
high impact exercise.
Though big claims are made regarding survival of
arthroplasty implant, with catchy statements like "joints
for life time" being common in media, high impact activities
can result in early failure of arthroplasties. Osteotomy
does have disadvantages. For example, pain relief is not as
predictable after osteotomy compared with a partial or total
knee replacement. Because you cannot put your weight on your
leg after osteotomy, it takes longer to recover from an
osteotomy procedure than a partial knee replacement. In some
cases, having had an osteotomy can make later knee
replacement surgery more challenging. Results from total
knee replacement and partial knee replacement have been
excellent, making knee osteotomy a less preferred procedure.
Nevertheless, it remains an option for many patients, since
the procedure is very economical as compared to
arthroplasty.
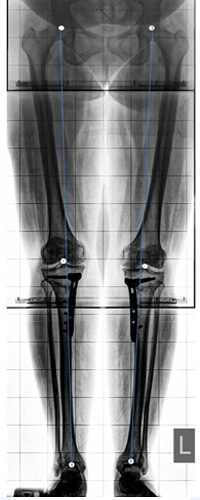
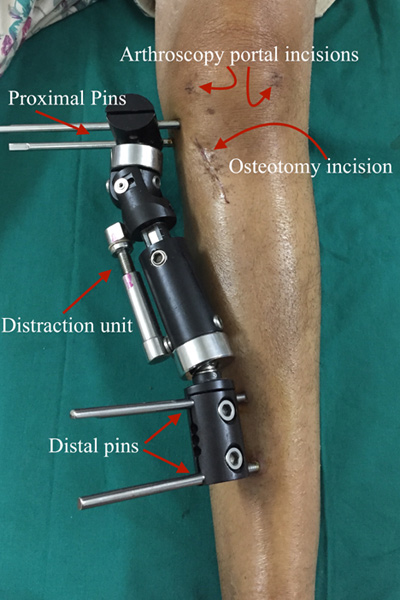
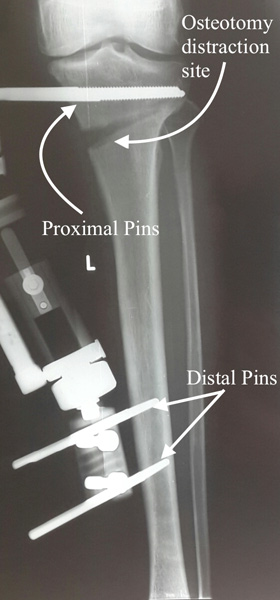
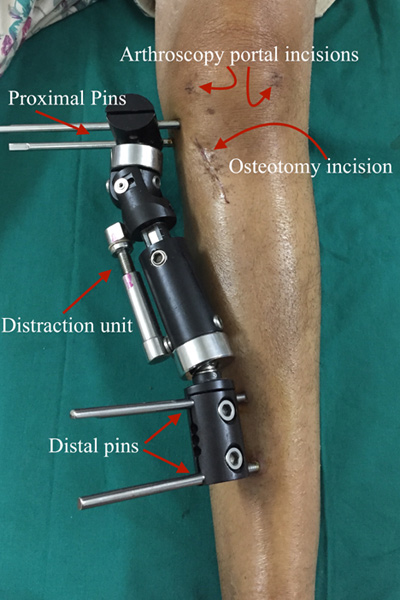
Procedure
High tibial osteotomy can be performed by open wedge or
close wedge technique. Both techniques have their own pros &
cons. We prefer open wedge technique with locking plate or
Ex-fix construct. Ex-fix HTO clamp being my personal
favorite, since it allows more precise control over the
final alignment. During this procedure two pins are fixed in
upper part of shin bone and two pins are fixed in lower part
of shin bone and oblique osteotomy is performed with hing at
proximal tibiofibular joint (outer side of proximal shin
bone). Distractor is attached to the pins fixed on shin
bone, which is gradually distracted over next few days. This
results in medial opening of the osteotomy, and shifts the
weight-bearing axis from medial compartment to lateral
compartment of knee. As the load is transferred to lateral
(healthy) compartment of knee and medial compartment is
distressed, this resulting in pain relief. Scientific
studies have documented growth of healthy cartilage one
eroded medial compartment of the knee joint.
Candidates for Knee Osteotomy
Knee osteotomy is most effective for thin, active patients
who are 40 to 60 years old, though we have successfully used
it in younger patients who had post-traumatic and
post-operative varus knee deformities. Good candidates have
pain on only one side of the knee, and no pain under the
kneecap. Knee pain should be brought on mostly by activity,
as well as standing for a long period of time. Candidates
should be able to fully straighten the knee and bend it at
least 90 degrees.
Your Surgery
Before Surgery
You will likely be admitted to the hospital on the day of
surgery.
Before your procedure, a doctor from the anesthesia
department will evaluate you. He or she will review your
medical history and discuss anesthesia choices with you.
We prefer regional anesthesia (spinal), so that you are
awake but your body is numb from the waist down. Your
surgeon will also see you before surgery and mark your
knee to verify the surgical site.
Surgical Procedure
A knee osteotomy operation typically lasts between 60 to
90 minutes. As a protocol, we routinely perform
arthroscopic debridement and micro-fracture in the same
sitting, unless there is a reason for not doing the same.
Arthroscopic debridement is a pen hole surgery in which
the knee joint is thoroughly examined from inside to look
for amount and kind of damage to the knee joint along with
removing any debris generated by the arthritic process.
Additional issues like meniscus tears are addressed and
microfractures are performed stimulate cartilage formation
in eroded medial femoral condyle. Following this, your
surgeon will make stab incisions on medial side of your
upper shin bone to fix to pins. HTO clamp in applied and
to pins are fixed in lower part of shin bone at distal
holes of clamp.
He will plan the correct site of the wedge using guide
wires under fluoroscopy control. With an oscillating saw,
your surgeon will cut along the guide wires to create an
osteotomy. HTO clamp is fixed in compression mode and
osteotomy wound in closed after confirming completeness of
osteotomy by distracting it once under fluoroscopy
control. In some cases, the wedge of bone is "opened" and
a bone graft is added to fill the space and help the
osteotomy heal. In this situation the osteotomy is fixed
with locking plate after correcting the alignment under
fluoroscopy control.
After the surgery, you will be taken to the recovery room
where you will be closely monitored as you recover from
the anesthesia. Following this you will then be taken to
your hospital room.
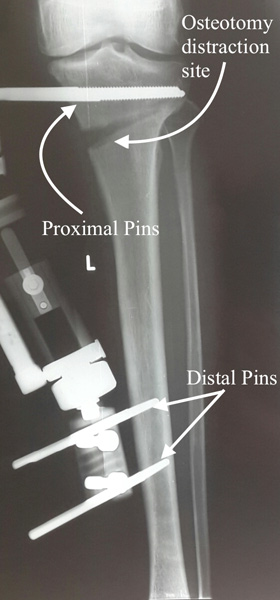
After Surgery
In most cases, patients stay at the hospital for 1 to 2 days
after an osteotomy. During this time, you will be monitored
and given pain medication. Your surgeon will explain you
exercises to strength thigh muscles, maintain knee ROM You
will most likely need to use crutches for several weeks. On
10th post-operative day, you will be explained distraction
technique. Distraction is carried out on daily bases for 3 –
4 weeks depending upon amount of deformity to be corrected.
X-rays will be taken at regular intervals so that your
surgeon can check how well the osteotomy is distracting.
When required distraction (as calculated pre-operatively) is
achieved, knee alignment is checked under fluoroscopy
control to confirm adequate correction of deformity. Once
the target is achieved, HTO distraction device is locked and
full weight bearing is allowed. You can walk with the help
of aids for next 4 weeks, when distractor is removed. During
rehabilitation, a physical therapist will give you exercises
to help maintain your range of motion and restore your
strength. You may be able to resume your full activities
after 3 to 6 months.
Complications
As with any surgical procedure, there are risks involved
with osteotomy. Your surgeon will discuss each of the risks
with you and will take specific measures to help avoid
potential complications. Although the risks are low, the
most common complications include:
- Infection
- Blood clots
- Stiffness of the knee joint
- Injuries to vessels and nerves
- Failure of the osteotomy to heal
Very rarely, a second surgery may be required, particularly
if the osteotomy does not heal.
Conclusion
Osteotomy can relieve pain and delay the progression of
arthritis in the knee. It can allow a younger patient to
lead a more active lifestyle for many years. Even though
many patients will ultimately require a total knee
replacement, an osteotomy can be an effective way to buy
time until a replacement is required.
Commonly asked questions?
Are there limitations on activity after an HTO?
Limitations after HTO are minimal among all the treatment
options for osteoarthritis knee i.e. Unicondylar knee
replacement, Total knee replacement and High tibial
Osteotomy. Limitations after joint replacement are important
since the bone cement interface can fail under extremes of
stress like running and jumping. In HTO its natural knee
joint whose alignment has been corrected to off load the
over loaded medial compartment. Since there is no artificial
component in the knee, you can treat your knee as original
or unaffected knee.
Will my knee be as good as normal knee?
Since HTO is usually done for OA it is not possible to
expect a completely normal knee when surgery and recovery
are complete. However, it is possible to return to whatever
activities can be tolerated within the limits of one’s own
residual level of pain and discomfort.
In general the HTO should severely slow down future further
development of degenerative osteoarthritic change and allow
improved but probably not completely pain free function
post-op.
If the OA is moderately severe at the time of the HTO, most
people will be able to delay the possible future knee
replacement by almost a decade.
Will I have a lot of pain after surgery?
Perception of pain varies from person to person. It is
present on first post-operative day; however, by 2nd
post-operative day it reduces to tolerable levels, which
will not require injectable analgesics. You will have
minimal pain by the time you are discharged.
How long will I be in hospital after the surgery?
We generally discharge all our patients next day afternoon.
Diabetic patients with not so good control of blood sugar
levels might have to extend hospitalization by one day.
Similarly pain management requiring injectable analgesics
can be another reason for delay in discharge.
How long does it take to achieve full correction of
alignment?
Your surgeon will provide you estimate time after surgery.
We routinely start distraction 10 days after surgery and
distract osteotomy @ 1 mm per day. Majority of patients
require 20 to 25 mm of distraction depending upon degree of
varus. With this calculation distraction ends at 30 to 40
days after surgery. This figure can vary from person to
person.
What do I do to care for the surgical wound and pin
tracts?
First dressing change is done on first post-operative day,
before discharging the patient. Second dressing is changed
at week’s interval. If any stitches are applied at osteotomy
site, they are moved on 12th post-op day. Osteotomy wound is
left open 14 days after surgery. Pin tracts need regular
care till the fixator is removed. All that one needs to do
is to clean the pin tracts with hospital spirit twice days
and apply betadine ointment over it.
Is swelling of knee joint a normal phenomenon?
Knee swelling is expected in early post-operative days. The
amount of swelling can be variable but often is quite
dramatic. The main reason for swelling is oozing from sites
of microfractures and osteophyte debridement, in addition to
some oozing from soft tissue sites. Due to the effect of
gravity, swelling is often noted to extend down to the foot
and ankle region (depending on the amount of time spent in
an upright position). Swelling may also be seen to
accumulate into the thigh if the leg is propped up for a lot
of the time in the first few days. A tensor wrap from foot
to thigh over the first few days can help to reduce some of
the immediate postoperative swelling. Ice packs should be
applied on knee to help reduce swelling. Your doctor may
prescribe for you an anti-inflammatory medication in the
early postoperative period, which can help control, some of
the swelling and is also an effective adjunct for pain
control. If you notice significant swelling in the calf or
thigh associated with a lot of posterior tenderness, this
may be a sign that a DVT (blood clot) is developing. This
warrants mentioning to your treating surgeon who will then
decide whether a Doppler ultrasound study is indicated to
help rule out a DVT.
What exercises should I be doing?
We recommend static quads exercise and ankle movement (for
calf muscles) form first port-op day. Range motion exercises
are started as tolerated from 7 days after the procedure.
Straight leg raising and abductor strengthening is
encouraged from 3 weeks onwards. After this individualized
exercise program is provided to the patient depending upon
his or her needs.
When can I go back to work?
Return to work is largely dependent on the type of work one
is returning to and also how long it takes for the acute
pain after surgery to settle. A general guideline would be
that most people returning to a sedentary type position
(e.g. Office work, shopkeeping) should be able to return
some time in the first 5 - 8 weeks post-op. There are many
factors that may allow some individuals to return to work
sooner than this i.e. rapid resolution of pain post-op, a
less pronounced swelling response, the ability to work from
home, the possibility of modifications being made in the
work environment i.e. ability to accommodate an initial
return on crutches. An individual returning to a more
physically demanding labouring type position would likely
return sometime between 4-6 months postoperatively.
Depending on the amount of distraction and the actual
physical demands of one’s job, the time to return could be
in some cases extended to even beyond 6 months. An earlier
return might be possible if modifications could be made in
the work environment to allow avoidance of heavy tasks and a
more gradual return.
When can I drive?
It is possible for patients to drive sooner if it has been
the left leg that has undergone surgery if there is access
to a vehicle with an automatic transmission. Driving should
be generally delayed until one is off narcotic pain
medication, and once reasonable mobility has returned. If
the left leg is the operative leg, most patients should be
able to drive approximately 6 weeks post-op. If on the other
hand, the right leg has been the operative leg, driving
should be delayed until full weight bearing has been
commenced and the patient is ambulating well i.e. usually
not before 3 months post-op.